Science Vs Spirituality in Nursing: Explanation!
Science and spirituality in nursing are essential components that work in harmony to provide comprehensive patient care. Nurses leverage the rigor of scientific knowledge and the compassion derived from spiritual understanding to treat patients holistically.
This integrated approach ensures that both the physical and emotional needs of patients are addressed, fostering an environment conducive to healing and comfort.
Science in nursing is grounded in evidence-based practice, which involves using the best available research and clinical expertise to make patient care decisions.
Spirituality, on the other hand, relates to a person’s beliefs, values, and experiences that give meaning to life, which can significantly impact health and well-being.
For example, a nurse might use scientific methods to manage a patient’s pain while also recognizing the importance of the patient’s spiritual needs, such as prayer or meditation, which could play a role in their overall recovery.
In the realm of nursing, the fusion of scientific methods and spiritual empathy is not just a philosophy but a daily practice that enhances patient-centered care and nurtures the soul of the healthcare community.

Key Takeaway
9 Aspects: Science Vs Spirituality in Nursing
| Aspect | Science in Nursing | Spirituality in Nursing |
|---|---|---|
| Focus | Empirical, evidence-based | Personal beliefs, values, and faith |
| Methods | Research, data, technology | Compassion, empathy, presence |
| Goals | Cure, symptom management | Holistic healing, comfort, peace |
| Approach | Objective, systematic | Subjective, individualized |
| Education | Medical and scientific knowledge | Cultural sensitivity, spirituality |
| Evidence | Quantitative, measurable outcomes | Qualitative, inner experiences |
| Ethical Considerations | Informed consent, confidentiality | Respect for diverse beliefs |
| Interactions | Diagnosis, treatment | Emotional support, spiritual care |
| Patient Experience | Physical well-being | Emotional and spiritual well-being |
The Role of Evidence-Based Practice

The role of evidence-based practice in nursing is essential for delivering high-quality, patient-centered care. Evidence-based practice integrates clinical expertise, patient values, and the best research evidence to make decisions about patient care.
In nursing, this approach ensures that interventions and treatments are based on the most current and reliable evidence, leading to better patient outcomes.
By critically evaluating research findings and applying them to individual patient needs, nurses can tailor their care to provide the most effective treatments.
This not only enhances patient safety and satisfaction but also fosters a culture of continuous learning and improvement within the nursing profession.
Transitioning to the subsequent section about ‘integrating spiritual care in healthcare’, it’s important to recognize that evidence-based practice forms the foundation upon which holistic and patient-centered care, including spiritual care, can be effectively integrated.
Integrating Spiritual Care in Healthcare
Integrating spiritual care in healthcare, while grounded in evidence-based practice, plays a crucial role in addressing the holistic needs of patients and promoting patient-centered care. It acknowledges that patients have spiritual needs that can impact their well-being and recovery.
Here is a table highlighting the key aspects of integrating spiritual care in healthcare:
| Aspects of Integrating Spiritual Care in Healthcare | Description |
|---|---|
| Holistic approach | Recognizing the interconnectedness of mind, body, and spirit in patient care |
| Patient-centered care | Tailoring care to individual spiritual beliefs and practices |
| Interdisciplinary collaboration | Involving chaplains, spiritual leaders, and healthcare providers in care planning |
| Ethical considerations | Respecting patient autonomy and religious preferences |
| Positive patient outcomes | Enhancing coping, resilience, and overall well-being |
Integrating spiritual care in healthcare aligns with the ethical principle of beneficence and contributes to a more comprehensive approach to patient care.
Ethical Considerations in Patient Care
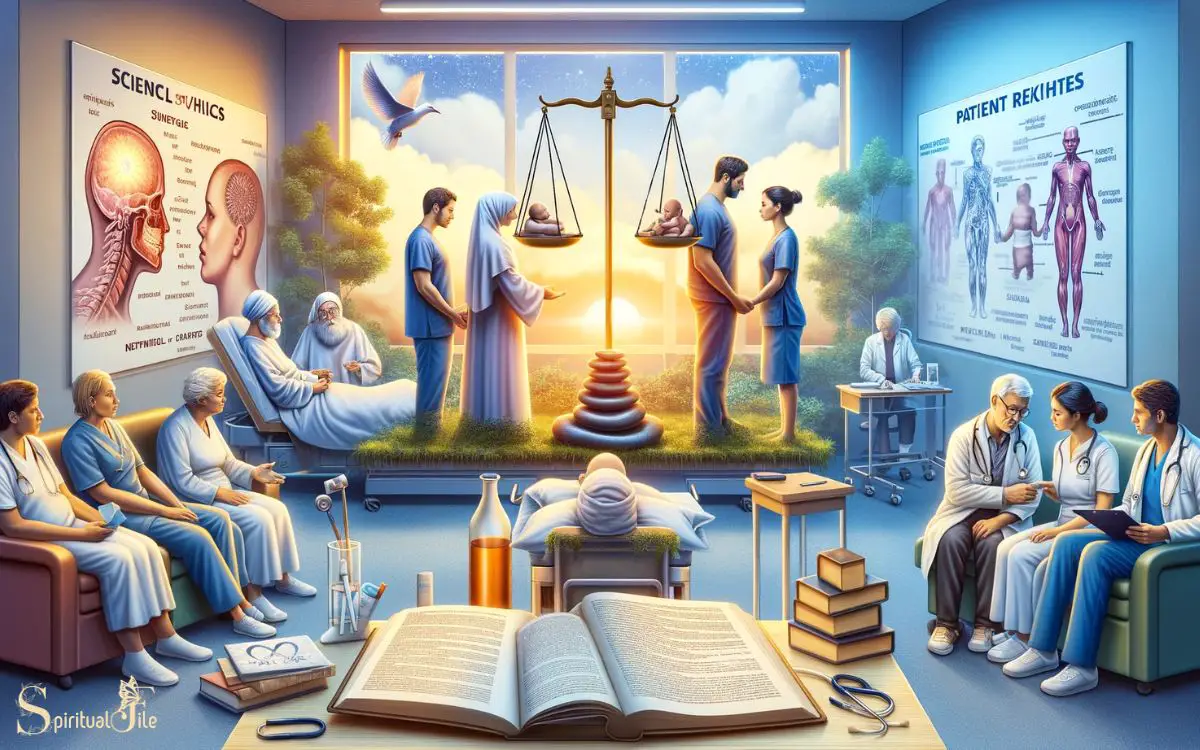
Ethical considerations in patient care play a fundamental role in guiding nursing practice and decision-making.
Nurses are often faced with complex ethical dilemmas, such as respecting patient autonomy, ensuring beneficence, and upholding justice.
It is essential for nurses to navigate these ethical considerations with integrity and sensitivity, taking into account the patient’s values, beliefs, and cultural background. This requires a deep understanding of ethical principles and the ability to apply them in real-life situations.
Additionally, nurses must also consider the legal and professional standards that govern patient care to ensure that their actions align with ethical and moral frameworks. By addressing ethical considerations in patient care, nurses can provide compassionate and respectful care that upholds the dignity and well-being of their patients.
Moving forward to discuss the next subtopic, let’s delve into the importance of balancing science and compassion in nursing practice.
Balancing Science and Compassion

Balancing science with compassion is essential in nursing practice to ensure holistic and empathetic patient care.
It is crucial for nurses to integrate evidence-based scientific knowledge with compassionate care to address not only the physical needs but also the emotional, mental, and spiritual well-being of patients.
The following table demonstrates the key aspects of balancing science and compassion in nursing:
| Science | Compassion |
|---|---|
| Evidence-based practice | Empathy and understanding |
| Clinical skills and technology | Patient advocacy and support |
| Critical thinking and analysis | Therapeutic communication |
By balancing these elements, nurses can provide comprehensive care that addresses the whole person, fostering healing and well-being.
This integration of science and compassion is fundamental in enhancing patient outcomes and overall satisfaction with care.
Transitioning into the subsequent section about ‘enhancing patient well-being through holistic care’, it is imperative to explore how integrating science and compassion leads to improved patient outcomes.
Enhancing Patient Well-Being Through Holistic Care
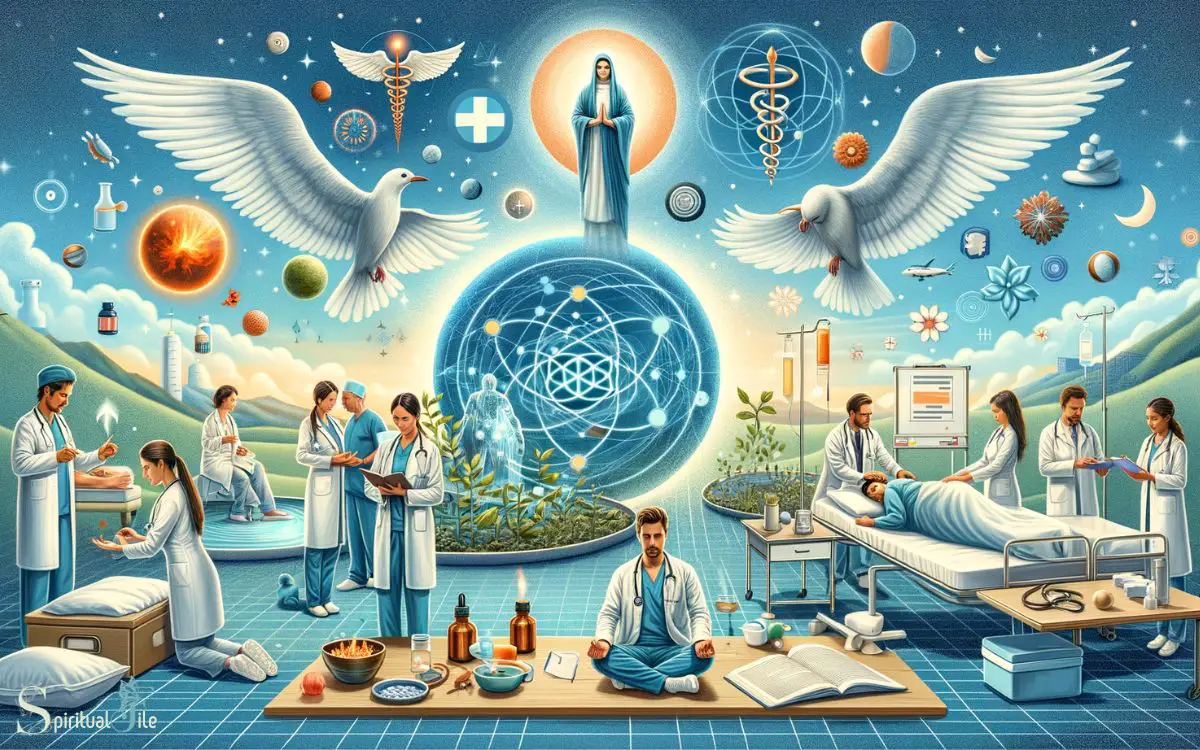
Transitioning from balancing science with compassion, enhancing patient well-being through holistic care involves addressing the physical, emotional, mental, and spiritual needs of patients to promote comprehensive healing and wellness.
Holistic care recognizes that patients are more than their physical symptoms; it considers the interconnectedness of the body, mind, and spirit.
This approach involves integrating conventional medical treatments with complementary therapies such as massage, acupuncture, and mindfulness practices.
By acknowledging the emotional and spiritual distress that illness can bring, healthcare providers can offer a more complete and personalized form of care. Holistic care empowers patients to actively participate in their healing process, fostering a sense of control and autonomy.
Ultimately, by addressing the patient as a whole, holistic care aims to improve overall well-being and quality of life.
How Can Science and Spirituality be Integrated in Nursing Practice?
In nursing practice, the integration of science, spirituality, and measurable facts can enhance the holistic care provided to patients. By embracing both evidence-based medicine and spiritual support, nurses can address the physical, emotional, and existential needs of patients, leading to improved health outcomes and overall wellbeing.
FAQ of Science Vs Spirituality in Nursing
How Does Spirituality Impact a Nurse’s Personal Beliefs and Values in Patient Care?
Spirituality impacts a nurse’s personal beliefs and values in patient care by providing a framework for understanding and addressing patients’ holistic needs.
It can influence their approach to healing, empathy, and ethical decision-making in healthcare settings.
What Are Some Common Misconceptions About Spirituality in Healthcare and How Can Nurses Address Them?
Common misconceptions about spirituality in healthcare include it being solely religious, irrelevant to modern medicine, or only for end-of-life care.
Nurses can address these by integrating holistic care, respecting diverse beliefs, and promoting open communication.
How Can Nurses Navigate Conflicts Between Evidence-Based Practice and a Patient’s Spiritual Beliefs?
When navigating conflicts between evidence-based practice and a patient’s spiritual beliefs, and collaboration with interdisciplinary teams to provide holistic care that addresses both physical and spiritual needs.
What Are Some Strategies for Effectively Communicating With Patients About Their Spiritual Needs and Beliefs?
Effective communication with patients about their spiritual needs and beliefs involves active listening, open-ended questions, and respectful dialogue.
It is essential to create a safe and supportive environment, acknowledging and integrating the patient’s spirituality into their care plan.
How Can Nurses Ensure They Are Providing Holistic Care That Addresses Both the Physical and Spiritual Needs of Their Patients?
Nurses can ensure holistic care by acknowledging patients’ spiritual needs, actively listening, and providing support.
Incorporating spiritual assessments, collaborating with chaplains, and respecting diverse beliefs are essential for addressing both physical and spiritual aspects of patient care.
Conclusion
The integration of spirituality in nursing care is essential for holistic patient well-being. According to a study by the National Institute of Health, 72% of patients believe that spiritual care is important in their healthcare experience.
The balance between evidence-based practice and spiritual care is crucial in providing ethical and compassionate patient care. By embracing both science and spirituality, nurses can truly enhance the overall well-being of their patients.